|
Report of invitational conference Clinical Guidelines
Amsterdam, November 10 and 11, 2006
|
|
|||
|
||||
|
The objectives of the conference were:
Friday November 10 The conference was opened by Antonio Lopes, chairman of the European Region of WCPT. He stressed the importance of clinical guideline development and collaboration between Member Organisations of the European region.
Low back pain guidelines On Friday morning similarities and differences between existing clinical guidelines Low Back Pain were discussed. Professor Maurits van Tulder introduced the multi-disciplinary European guidelines for acute low back pain, while dr. Erik Hendriks and dr. Anne Jackson presented the physiotherapy specific low back pain guidelines in the Netherlands and UK respectively. The multi-disciplinary guideline appeared to be described at a general level, to be used by all health care professionals. The physiotherapy guidelines were more specific and closer to daily practice for the physiotherapist. The physiotherapy guidelines showed for the most part similarities in recommendations, although some (smaller) differences were apparent, due to differences in current practice between UK and the Netherlands, but may also be caused by different interpretation of the evidence. Professor Rob de Bie, as chair of the session, showed some of the benefits and pitfalls of using evidence in clinical guidelines. Although evidence from research is essential for developing guidelines, only relative small parts of guidelines are really based on evidence. More research is needed to fill the gaps. Also, the use of evidence to formulate recommendations may be different due to national and or local circumstances. Part of discussion was about the difficulty to implement clinical guidelines. Physiotherapists are not always eager to use evidence to change their treatment of patients.
Conclusion of the morning session was that multi-disciplinary guidelines, as general ‘mother’ guideline for all health care professionals are useful instruments to describe the full range of care and to stimulate collaboration between professionals. Physiotherapy specific guidelines are very useful to support and guide daily physiotherapy practice. Implementation of guidelines is still a major issue in most countries, because to change professional behaviour towards evidence-based practice requires much effort.
Collaboration and implementation During the afternoon session short presentations were used to introduce involvement of physiotherapists in multi-disciplinary guideline development (Judy Mead), a plan of action for guideline development in Nordic countries (Heidi Anttila), Review of CSP guideline development programme in the UK (Ralph Hammond), adaptation of existing guidelines (Philip van der Wees), and implementation of existing guidelines in Lebanon (Claude Maroun). The introductions were used as warming-up for interactive discussion in subgroups. Three themes were discussed: a. Collaboration between guideline developers in the European Region of WCPT
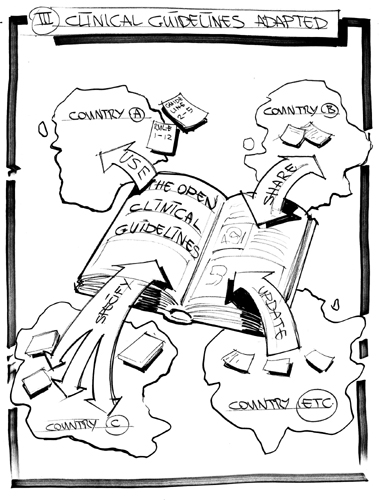
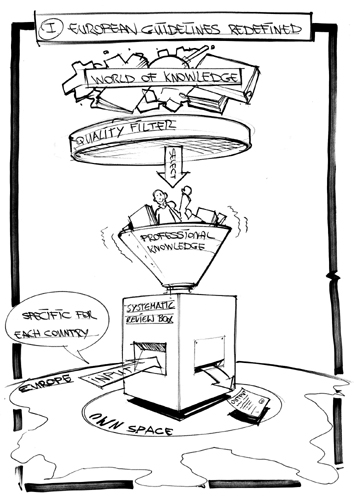
The subgroup recommended that information should be available about development of clinical guidelines by member organisations of the European Region of WCPT. When information is available, Member Organisations may be able to agree to share work, primarily by doing joint systematic reviews. Based on the collected evidence, each Member Organisation can use the evidence to formulate recommendations for their own specific national circumstances. b. Adoption and implementation of clinical guidelines for use at national or local level.
The recommendations form the subgroup were to prepare a position paper about the use of clinical guidelines by Member Organisations of WCPT, individual physiotherapists and government. The position paper can be used to facilitate the understanding and implementation of clinical guidelines. Furthermore the European region of WCPT should seek collaboration with the ADAPTE group (for a project to test their protocol for adaptation of guidelines). Possible projects are testing the ADAPTE manual in Germany (by ZVK), and to explore the use of the manual by the Nordic countries. c. Involvement of member Organisations in multi-disciplinary guideline development at national level.
To enhance physiotherapy involvement in multi-disciplinary guideline development, the subgroup recommended to facilitate access to clinical guideline across Europe by keeping the database of the European Region of WCPT up to date. The European Region of WCPT should become a member of the Guidelines International Network (GIN).
Saturday November 11 The theme of the Saturday program was ‘challenges for the future’. Brenda Myers (secretary general of WCPT) opened the session and noticed that to support Member Organisations will be the main challenge for WCPT. Worldwide several topics need to be addressed: level of education, stimulation of direct access, relation with other medical professions. Professor Paul Helders (Netherlands) gave an overwiew of developments in physiotherapy claiming that ‘you don’t have a future if you don’t have a past’. He showed the paradigm shift in physiotherapy from disablement to enablement, leading to a focus on daily functioning of the patient. Physiotherapists should be proud of their profession and should read, publish and discuss the developments. The swift developments in physiotherapy was confirmed by professor Ann Moore (UK) who showed the increase of PhD physiotherapists from 6 in 1996, while UK has currently 200 PhD’s. The future of physiotherapy in the UK will depend on a good level of education for both professional and scientific performance. In the afternoon dr Lisa Saladin (USA) showed some of the current problems in the USA. Although direct access is regulated by law in most states, many insurance companies do not reimburse direct access. Also collaboration between physicians and physiotherapists is becoming more difficult, because many physicians are owner of physiotherapy clinics which reduces the autonomy of the physiotherapists. The lack of evidence in physiotherapy and bias of published evidence was topic of discussion in the presentation of professor Rob de Bie (Netherlands). Research is expensive and physiotherapy is not sexy enough for financiers. Research is not always of high quality and may be difficult to apply. Continuing education is essential for implementation of evidence in daily practice. Dr. Gro Jamtvedt (Norway) showed the massive amount of research in the field of physiotherapy. Almost 8,000 RCT are currently available, compared to 2,500 in 2002. But the availability of evidence does not necessarily reflect daily practice. Her statement was that the patient should be more involved in clinical decision making, based on the definition of evidence based practice. The last presenter of the day was dr. Bas Haring (Netherlands), who showed his views for the future as a philosopher. He hypothesised that developments in physiotherapy will be gradually, and not in huge steps. Physiotherapy is not about dramatic developments like cardiac surgery, but more like a growing body of knowledge as in psychiatry. |
||||


 Print this page
Print this page Recommend this page
Recommend this page Report defect link
Report defect link